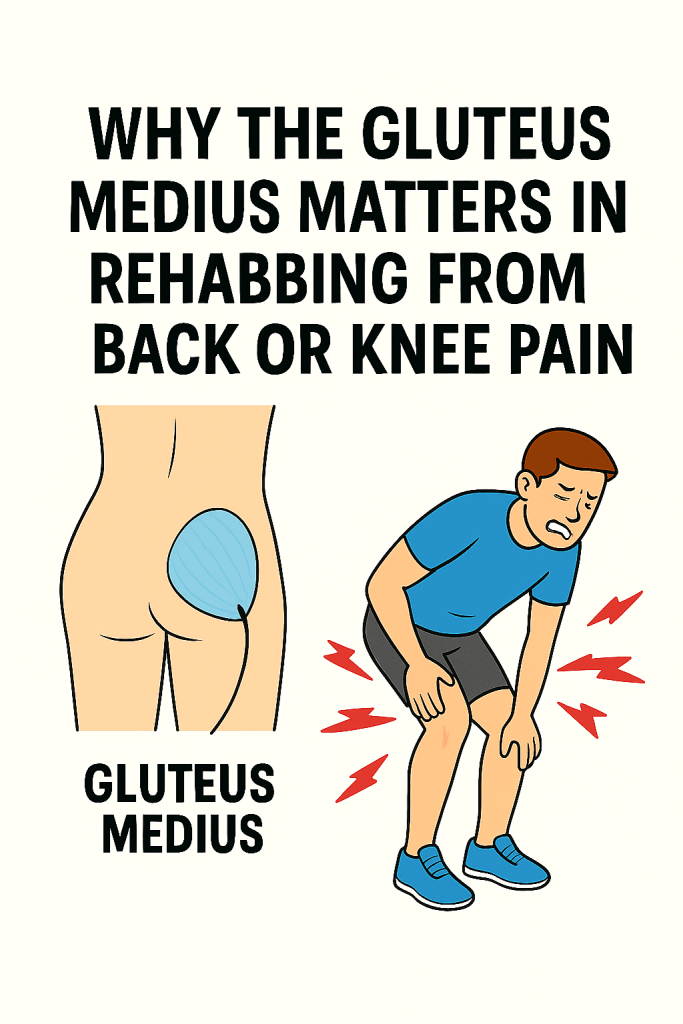
Knee pain and low back pain often trace back to the same culprit: poor gluteus medius function. When this muscle isn’t firing well, the knee can collapse inward (valgus), stressing the joint and contributing to patellofemoral pain. At the same time, an underactive glute medius fails to stabilize the pelvis, forcing the lower back and surrounding muscles to take on extra work—often aggravating pain instead of easing it.
That’s why the gluteus medius is such a key player in both injury rehab and long-term resilience. Let’s look at what it actually does, and which exercises best restore its strength and stability.
🔑 Key Functions
Hip Stabilization (especially when standing on one leg)
The gluteus medius helps keep your pelvis level when you walk, run, or stand on one leg.
Without it, your pelvis would “drop” on the unsupported side—a condition called Trendelenburg gait.
Lateral Stability & Balance
It acts like a side anchor, keeping your hips, knees, and ankles in good alignment.
This protects against wobbly knees, ankle rolling, and inefficient force transfer when moving.
Hip Abduction
Moving your leg out to the side (like in side steps or kicking outward) is primarily the job of the glute med.
It also helps rotate the hip outward and inward depending on leg position.
Joint Health & Injury Prevention
A weak glute med often shows up as knee pain, IT band issues, or hip discomfort.
Runners, lifters, and athletes especially rely on it to prevent overloading other muscles and joints.
Athletic Power & Efficiency
Strong glute medius = better agility, cutting, lateral shuffling, sprint mechanics, and force transfer.
It’s a hidden powerhouse for acceleration and deceleration.
👉 In short: the gluteus medius keeps you upright, balanced, and protected, whether you’re just walking down the street or cutting hard on the basketball court. It’s a stabilizer first, mover second—and that’s what makes it so essential.
🏋️ Exercises to Strengthen Your Glute Medius
Here are three of the most effective exercises to strengthen your gluteus medius. They’re simple, but if you load or sequence them right, they hit hard:
1. Side Plank with Hip Abduction (Hold Variation)
How: Start in a side plank on your elbow. Lift the top leg just a few inches and hold it there for 5–10 seconds before lowering.
Tips:
- Keep hips stacked and core engaged so you don’t rotate forward or backward.
- Focus on stability, not just swinging the leg.
Why: Builds glute med strength while training it in its stabilizing role, which carries over more directly to real-life movement.
Note: Variations like clamshells with a band or banded side planks are also great for learning to activate and stabilize the glute med.
2. Banded Lateral Walks (a.k.a. Monster Walks / Side Steps)
How: Place a resistance band around your thighs (just above knees or ankles). Get into an athletic quarter-squat and take wide steps sideways.
Tips:
- Keep constant tension on the band (don’t let your feet snap together).
- Stay low to keep glutes engaged.
Why: Teaches hip stability and strengthens glute med under load—fantastic for runners and athletes.
3. Single-Leg Glute Bridge / Hip Thrust
How: Lie on your back, one foot planted, the other lifted. Drive through your planted heel to lift hips off the ground.
Tips:
- Actively keep hips level (don’t let one side sag).
- Squeeze glutes at the top, control on the way down.
Why: Forces the glute med to stabilize pelvis while the glute max drives extension—mimics real-life one-leg stance mechanics.
Note: For those working with a coach or therapist, more advanced drills like the DNS star can build even deeper coordination, but most people will benefit from starting with these simpler exercises first.
⚡ Bonus progression: Once you’ve mastered these, add Bulgarian split squats or single-leg Romanian deadlifts. They hit the glute med hard as a stabilizer in functional patterns.
✅ Conclusion
Strong gluteus medius muscles don’t just build athletic power — they protect your joints, improve balance, and keep everyday movement smooth and pain-free. Whether you’re rehabbing from low back or knee pain, training for sport, or just looking to feel stronger on your feet, a little focused glute med work goes a long way.